The Importance of Patient Information

Where do patients find trustworthy and reliable information when they have a suspected adverse drug reaction? A just published paper, by my colleagues and I, gives some insight:
Seeking information when experiencing a symptom which could be a side effect from a medicine is a common strategy, potentially predicted using the SECope instrument, but not the MBSS. Doctors, regarded as trustworthy sources of information, are frequently used when such effects occur. However, their limited accessibility could contribute to high use of the internet as an alternative or additional information source. PILs were not considered as trustworthy by many people using regular medicines, but were nonetheless used frequently due to easy accessibility. Further work is needed to identify how these documents, ubiquitous in many countries, can be improved to increase trustworthiness. Reasons for not seeking information from pharmacists, despite their accessibility and trustworthiness, also need investigation.
One of the side issues in the paper is the confidence patients had that their suspected adverse drug reaction was caused by the medicine. Over 90% of patients were confident about the association, enabling them to take action, such as contacting their GP. The consequences of the adverse drug reactions included admission to hospital (8.8%) and serious enough to affect their daily activities.
This is yet another reminder of the harm medicines inherently hold, the importance of listening to patients, and the crucial role that providing accessible trustworthy information they can use to make decisions has.
O’Donovan B, Rodgers R, Cox A, Krska J. Use of information sources regarding medicine side effects among the general population: A cross-sectional survey. Primary Health Care Research & Development 2019; 20: E153. doi:10.1017/S1463423619000574
Cambridgeshire Methotrexate Toxicity Report
In April of 2000, a patient died following an avoidable presribing mistake. A once weekly dose of methotrexate was prescribed daily. A speaker at the Royal Pharmaceutical Society’s Conference last Sunday reminded me that the excellent Cambridgeshire Health Authority report of this incident used to be kept on my old website, since the original NHS website had disappeared.
For the purposes of keeping this important example in the public domain, I have put the PDF of the report on this site.
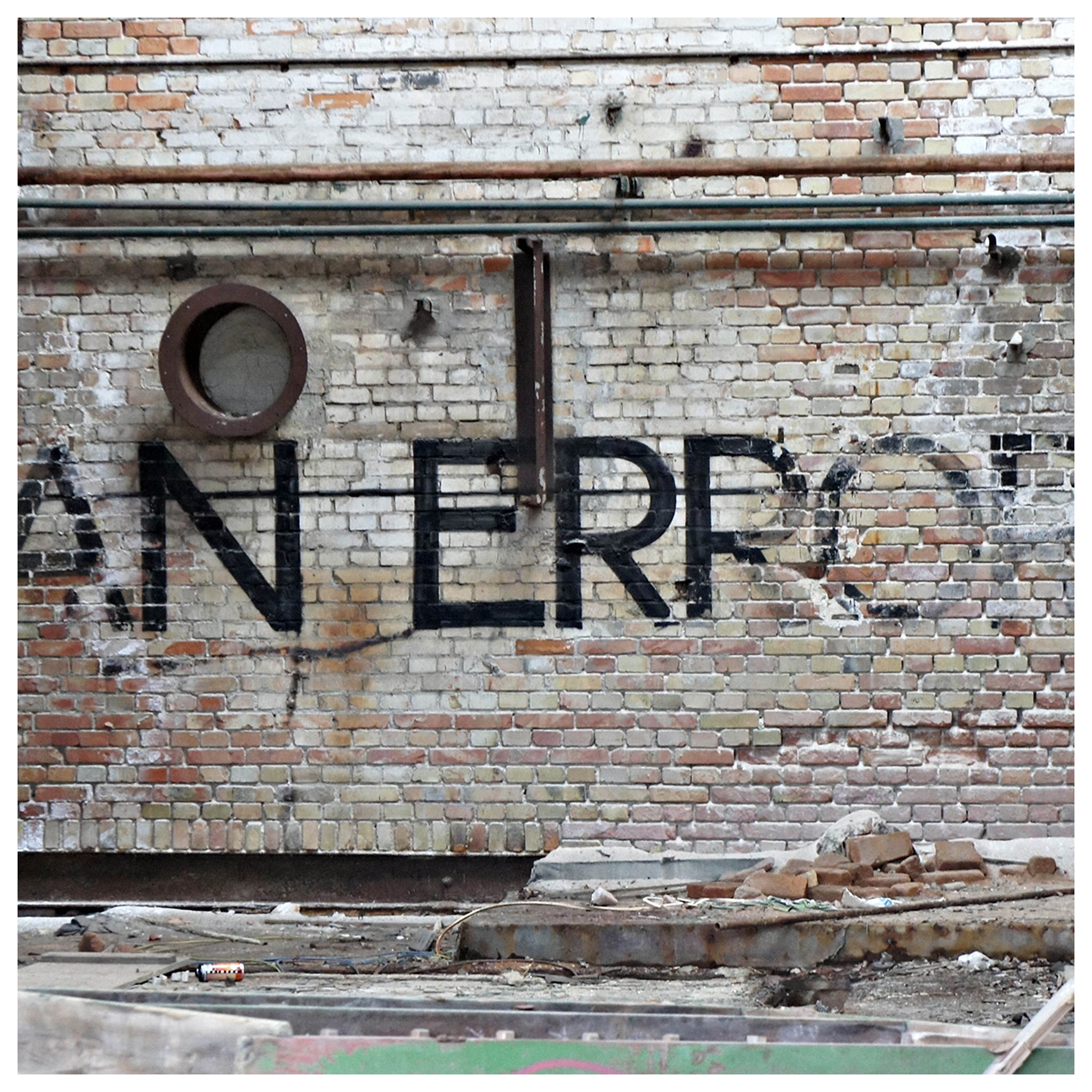
METHOTREXATE TOXICITY AN INQUIRY INTO THE DEATH OF A CAMBRIDGESHIRE PATIENT IN APRIL 2000
Photograph: “error” by strange little woman on stream. Attribution 2.0 Generic (CC BY 2.0)
Shortages and Shifts

Medicines shortages are more than the abscence of medicines for patients. Prescribers will prescribe alternative drugs, which may be less safe. As a brief follow-up to a recent post on drug shortages, I looked at the outcomes following a shortage of naproxen (a non-steroidal anti-inflammatory drug – NSAID) using Open Prescribing Data. It appears that patients have been switched, at least in part, to other NSAIDs that carry a greater risk of cardiovascular, renal, and gastric adverse effects. I have posted this in a BMJ rapid response to Ferner et al’s piece on drug shortages:
From September to December 2018, prescribing of naproxen in English CCGs fell from 581,927 items to 480,171 items (a 17.5% fall). In September 2018, naproxen prescribing cost £1,495,703 – by January 2019 it had risen to £9,206,903, despite reduced prescribing. Apart from these financial costs, there was a regrettable shift in prescribing, as the proportion of NSAIDs with greater risks of cardiovascular, gastrointestinal, and renal adverse effects rose. The “Number of prescription items for all NSAIDs excluding ibuprofen and naproxen as a percentage of the total number of prescription items for all NSAIDs” rose from 20% in September 2018 to 24% in January 2019.
Given the current problems with shortages, care needs to be taken when substituting medicines. Those who write guidelines, or issue prescribing advice, should consider second line therapies in the event that the first line drug is unavailable.
UPDATE: December, this is now a published letter at the BMJ
Photograph: “White round pills on blue background” by Marco Verch. Attribution 2.0 Generic (CC BY 2.0)
Medication Safety - Call for Papers

Pharmacists are involved in all areas of the development, manufacture, supply, and monitoring of medication. They work in pharmacies, hospitals, the pharma industry, medicines regulators, and increasingly, in the UK, in General Practice. They are ideally placed, and trained, to help reduce the major burden of drug-related harm caused by the widespread use of inappropriate medicines.
As part of the need to develop the evidence base for the contribution pharmacists can make in this area, including how pharmacists can work with patients, I am co-editing a special themed issue of the International Journal of Pharmacy Practice.
there will be a special issue of the IJPP in 2020, containing papers relating to the contribution of pharmacists to medication safety. We welcome submission of papers describing innovative approaches to enhancing medication safety, or rigorous evaluation of existing validated medication safety tools. Papers addressing the contribution of pharmacists to communication with patients and carers and multidisciplinary attempts to reduce the harms of medications are also encouraged. Please submit papers by 31st January 2020, using our online system, and use the tick box provided to indicate that you wish the paper to be considered for inclusion in the special issue. Accepted papers are available immediately on our web pages via ‘early view’. The print version of the special issue is scheduled for the second half of 2020.
The rest of the details of the call for papers can be found here.
Photograph by Ivan Radic. Attribution 2.0 Generic (CC BY 2.0)
Brexit and Drug Shortages

Here’s a short piece on the potential effects of Brexit on the supply of medicines I wrote for the University of Birmingham. I set these concerns against the underlying problems around drug shortages, and was considering a no deal Brexit. Any deal is likely to further mitigate the problems of any Brexit.
The effects of Brexit, and consequences of attempts to mitigate those effects, are difficult to predict. Any evaluation is complicated by the baseline rates of drug shortages caused by other factors. Media reports of medicine shortages and their causes in the aftermath of Brexit may be influenced by the polarisation seen in the wider Brexit debate. What is clear though, is that even if government attempts to avoid medicine shortages are entirely successful, and supply chains adapt rapidly to post-Brexit changes, the underlying structural causes of medicine shortages will affect the supply of medicines for years to come.
Photograph Banksy does Brexit by Dunk. Attribution 2.0 Generic (CC BY 2.0)